

Affiliations
ABSTRACT
Disc herniation of lumbar spine is common but it rarely presents at the intradural location. As for any disc herniation, patient undergoes the same clinical and radiologic examinations. However, the surgical excision is way more challenging. To remove the intradural disc material, a formal durotomy is required, which needs to be followed by dura repair. Here, we present three of such cases that were treated and their outcome is summarised. The spine surgeons need to be prepared for such operative findings and ensure water-tight seal of the dura following excision of the pathological disc material.
Key Words: Lumber intradural disc herniations, Durotomy, Discectomy, Degenerative disc disease.
INTRODUCTION
Disc herniation of lumbar spine is common. One of the rare presentations of the lumbar disc herniation is intradural disc.1 Therefore, thorough assessment is essential in cases of prolapsed intervertebral lumbar disc cases as the neuro-spine diagnostic imaging, i.e. magnetic resonance imaging (MRI) is unable to effectively depict the rare intradural presentation.2
Intradural disc prolapse is a rare presentation and the surgical excision of this entity is more cumbersome. Incising dura and subsequent water-tight repair with very fine suture is essential and requires good equipment and surgical experience. Therefore, preoperative planning is necessary. It is recommended that thorough assessment of preoperative imaging must be done to expect the condition preoperatively and then postoperative histopathological analysis should be performed to rule out other entities such as spinal tumours postoperatively.
Here, we present three such cases of intradural lumber disc herniation that were treated and their outcome is summarised.
CASE 1:
A 50-year male had been suffering from lower back pain radiating to both lower limbs alongside numbness, more marked on the right side, for the last 6 months. He also had perianal and right foot numbness.
On examination, power in quads and hams was 4/5 on right side, whereas bladder and bowel control were lost. Lasegue test (straight leg raise) was 45˚ on right and 60˚ on left. MRI revealed L5-S1 central disc prolapse, more towards the right side (Figure 1). During the procedure, disc was intradural and adherent to the dura from inside, though no dural rent was evident. Intraoperatively, hypertrophied ligamentum flavum was also observed. Thus, laminectomy was done and disc was removed after opening the dura. Subsequently, dural closure was done with 5-0 polypropylene suture. Disc was evident on histopathological analysis along with evidence of chronic inflammation. Postoperatively, the patient was followed for 1 month. Improvement in pain and power was noted, but bladder and bowel loss did not improve.
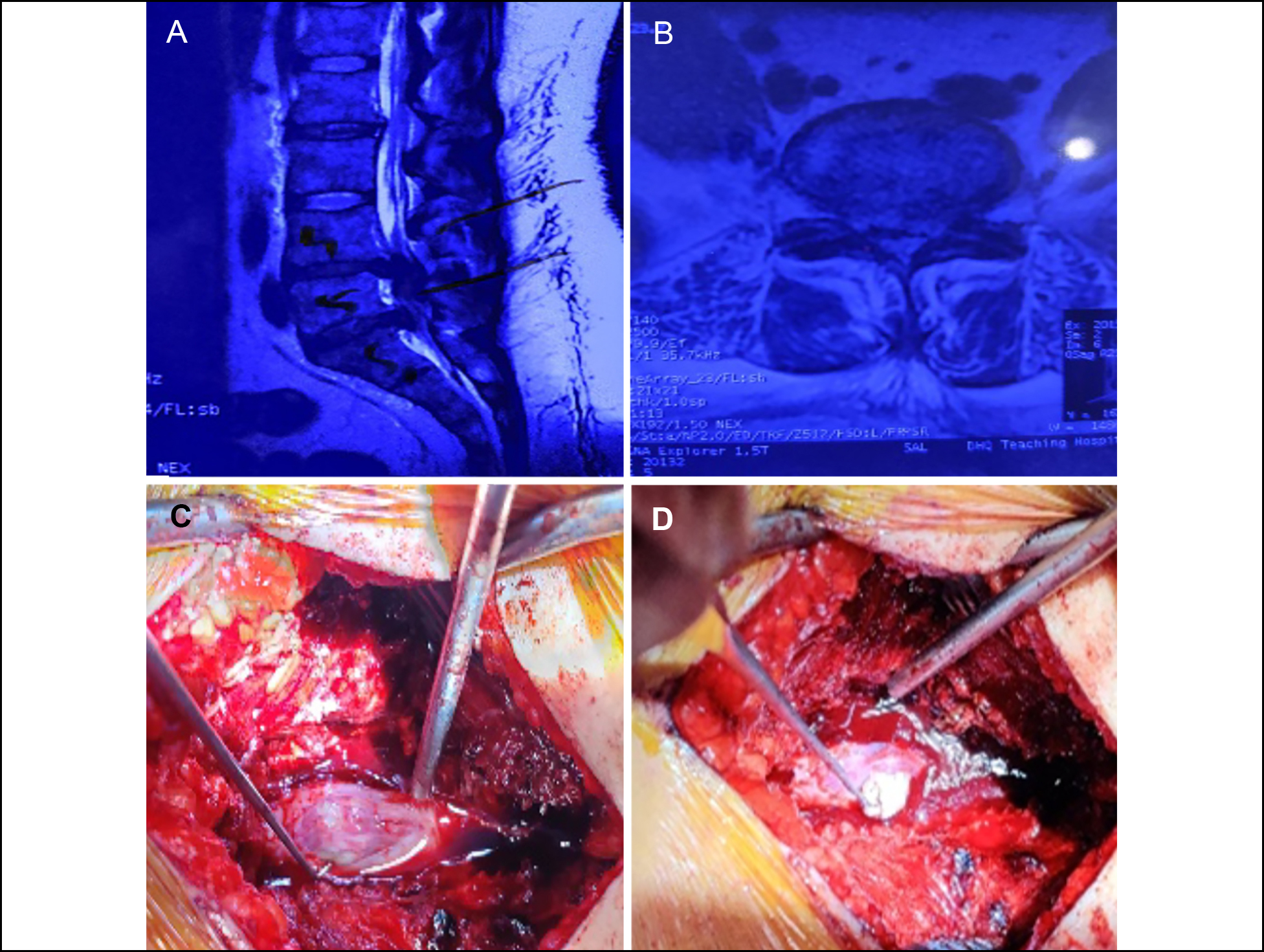 Figure 1: (A, B) MRI films showing prolapsed intervertebral discs. (C, D) Sequential pictures showing durotomy and removal of the intradural disc.
Figure 1: (A, B) MRI films showing prolapsed intervertebral discs. (C, D) Sequential pictures showing durotomy and removal of the intradural disc.
CASE 2:
A 22-year male who had been suffering from lower back pain with right lower limb radiation, alongside perianal numbness for 2 months presented to the outpatient department (OPD). He also had urinary and fecal incontinence for the last 1 week. On examination, power in right lower limb was 3/5. All the lower limb dermatomes were intact and planters were down-going. Lasegue test was 45˚ on right and 80˚ on left. MRI showed L4-L5 disc prolapse (Figure 2, A and B). During the surgical procedure, disc was intradural and a dural rent was evident. Thus, laminectomy was done and disc was removed after opening the dura (Figure 2, C and D). Subsequently, dural closure was done with berriplast and fibrin glue. Histopathological analysis confirmed degenerated disc alongwith the evidence of chronic inflammation. On one month follow-up, patient’s pain improved but power and bladder-bowel incontinence were same as before.
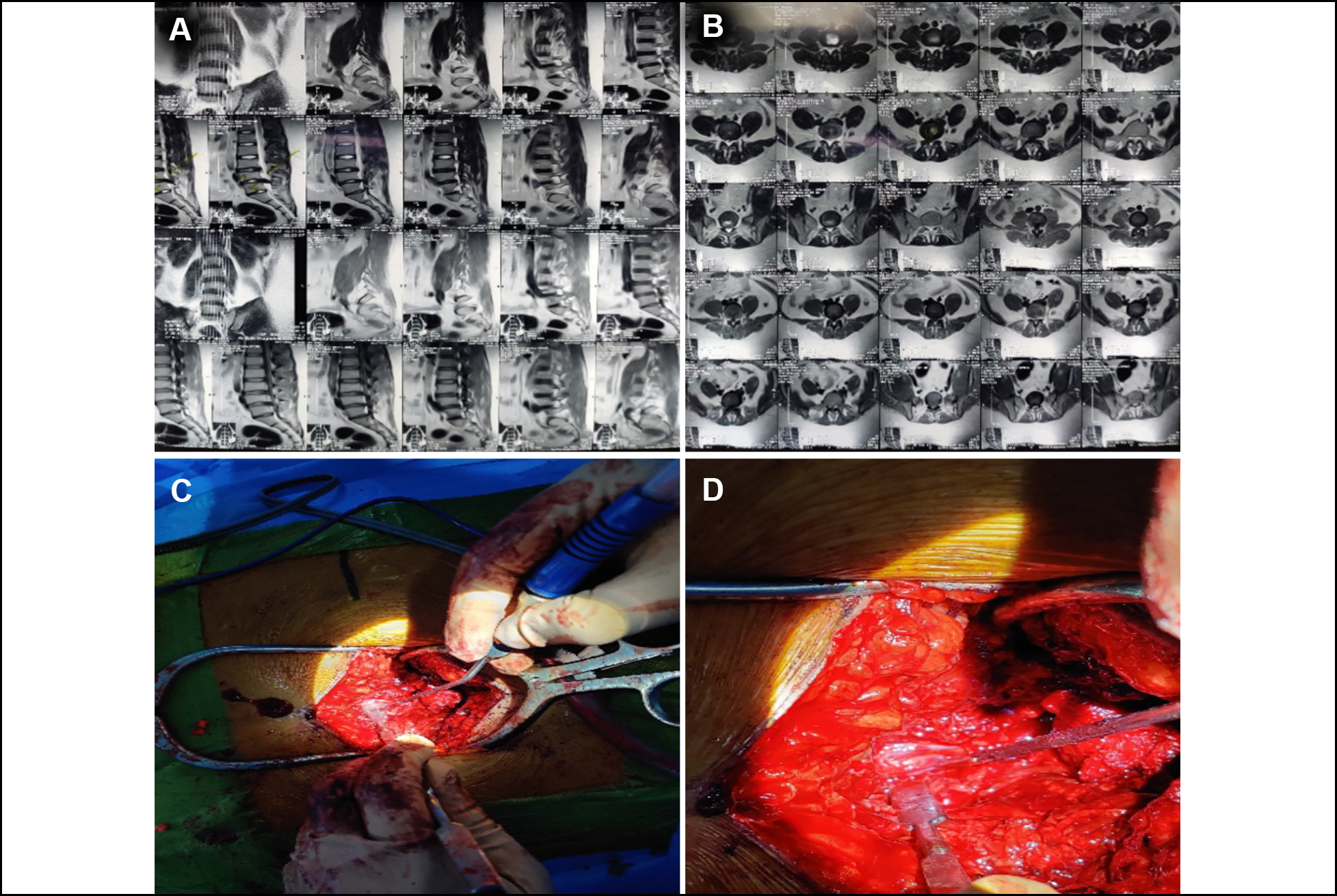 Figure 2: (A) and (B) show prolapsed intervertebral disc (PIVD) L4-5 on an MRI. (C) and (D) depict the dissection steps.
Figure 2: (A) and (B) show prolapsed intervertebral disc (PIVD) L4-5 on an MRI. (C) and (D) depict the dissection steps.
CASE 3:
A 37-year female, who had been suffering from lower back pain with bilateral lower limb radiations alongside numbness for the last 7 months visited OPD. On examination, all myotomes and dermatomes of both lower limbs as well as bowel and bladder functions were intact. Lasegue test was 45˚ on the right and 60˚ on the left. MRI showed L5-S1 disc herniation (Figure 3A). During the procedure, disc was intradural and adherent to the dura from inside, though no dura rent was evident. Hence, laminectomy was done and disc was removed after opening the dura, alongside left side root decompression (Figure 3, B and C). Subsequently, dural closure with 5-0 polypropylene suture was performed. On one month follow-up, she reported significant improvement in pain and neurology was intact on examination.
Patients were reviewed at 4 and 6 weeks postoperatively. Pain was settled and had no signs of local or systemic complications. On examination, neurology symptoms improved but bladder and bowel functions were not recovered in the patients who had incontinence preoperatively. Nonetheless, patients were mobilised and back to their normal daily activities by 3 weeks postoperatively.
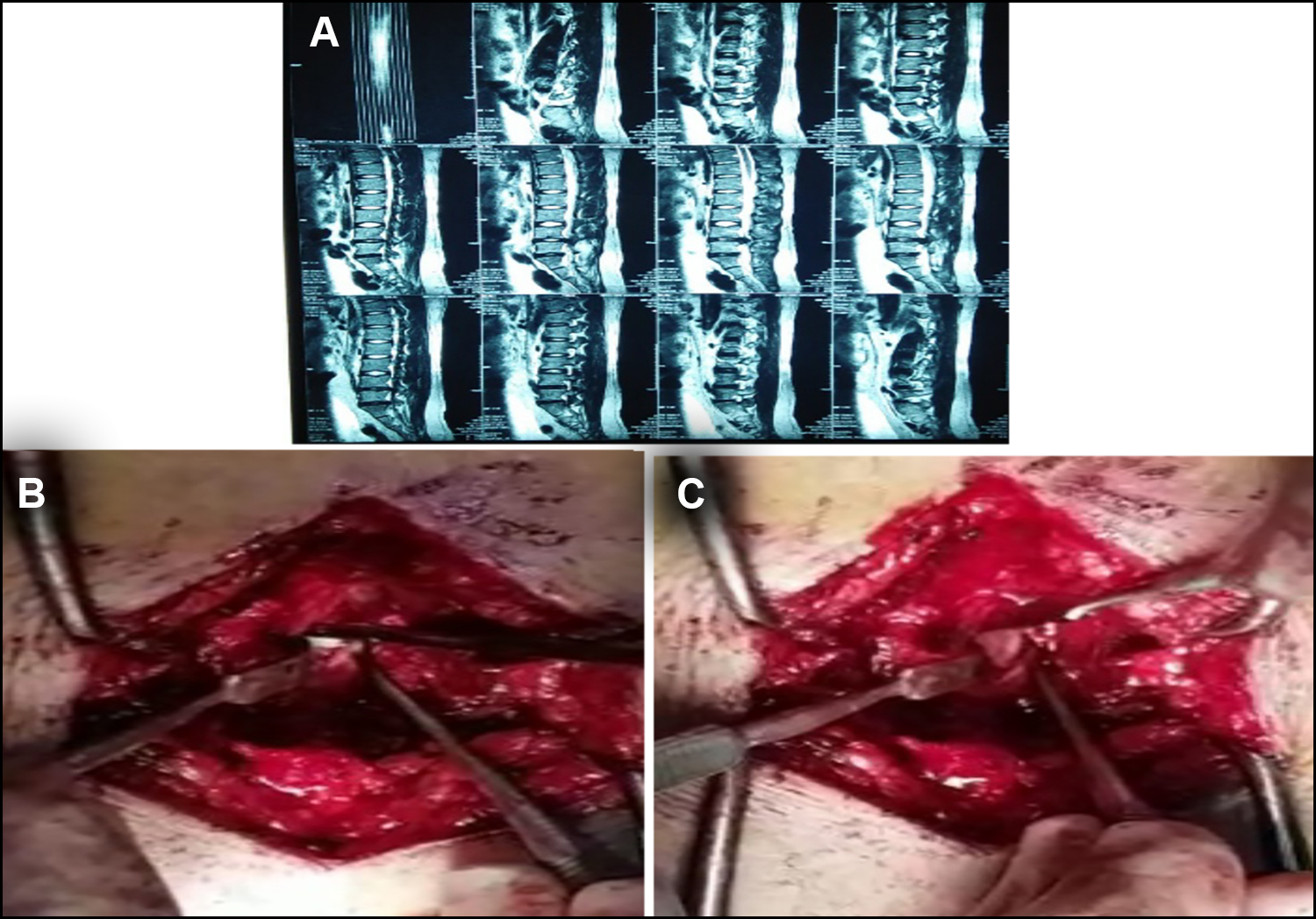 Figure 3: (A) shows prolapsed intervertebral disc (PIVD) L4-5 on an MRI. (B) and (C) depict the dissection steps during the removal of the disc.
Figure 3: (A) shows prolapsed intervertebral disc (PIVD) L4-5 on an MRI. (B) and (C) depict the dissection steps during the removal of the disc.
DISCUSSION
Prolapsed intervertebral disc (PIVD) is a very common entity in spine surgery, with published lifetime incidence of 13% to 40%.1 The disease causes significant morbidity and is a cause of huge socioeconomic burden; thus, best practice guidelines for diagnosis and management are well formulated. However, the intradural disc herniation (IDH), also termed as transdural herniation is not as common. This rare condition is usually indistinguishable from the extradural presentation preoperatively, and poses a challenge to the surgical team. Almost 92% of intradural disc presentations are at lumbar region, making it a 0.26 to 3% of total lumbar disc herniations. Among these, lower lumbar levels contribute most to the incidence: 55% at L4-5, 16% at L3-4 and 10% at L5-S1.3 IDH is four times more common in males and mostly presents in 5th to 6th decade of life.4
Though the exact aetiology is unknown but various theories have been put forward to explain the extrusion of nucleus pulposus within the annulus fibrosus and its subsequent migration through posterior longitudinal ligament and dural membrane to reach the intradural site. A theory suggested that chronic inflammation and subsequent adhesions that follow degeneration of disc result in erosion of dura and subsequent intradural migration of the disc material.5 Another explanation is that chronic compression caused by a variety of pathologies as postoperative or congenital stenosis causes thinning of dura and subsequent IDH.3,6
Preoperative identification of IDH can help prevent prolonged surgical procedure and indecision during the procedure, but preoperative imaging is rarely helpful in the diagnosis.7 Plain radiographs do not help at all, whereas, epidural gas around a sequestrated disc on CT scan may be of help as reported by Kobahashi et al. in their study.8 MRI, considered as a gold standard for neuro-imaging, has been shown by Nam et al. to have predictive accuracy on the basis of multiple findings associated with IDH.9 Among these, from most to least predictive are Y- sign on the ventral dura (PPV = 99.02%, NPV = 15.82%), beak-like shape (PPV = 98.73%, NPV = 18.8%), disc material beyond the PLL (PPV = 98.53, NPV = 15.85%), discontinuity of PLL (PPV = 98.34%, NPV = 25.28%), calcification or ossification of the disc material (PPV = 97.68%, NPV = 11.86%) and ill-defined margins (PVV = 97.51%, NPV = 15.18%). An abrupt discontinuity of the posterior longitudinal ligament is the most specific sign.9 Similarly, gadolinium-enhanced study can help to tell IDH apart from tumours or infections as IDH appears as an isointense mass with ring enhancement caused by contrast uptake by surrounding neovascularised granulation tissue. Another finding noted in T2-weighted imaging is “Y-sign”, caused by splitting of ventral dura line.2,10 Despite all these aforementioned details, IDH is mostly misdiagnosed. Thus, except for gadolinium-enhanced MRI in carefully selected patients, IDH is an intraoperative diagnosis.9
Surgical management of the entity varies from laminectomy and disc excision after durotomy to posterior interbody fusion and fixation. Interbody fusion is effective for prevention of recurrent disc disease.8 But, the matter of dura repair has been argued upon in the literature. Pedaballe et al. reported that the primary repair of ventral dural rent is necessary to prevent postoperative dural leak.7 On the other hand, Serikyaku et al. reported that ventral durotomy in 16 cases of IDH was not repaired and none of the patients developed CSF leak, postoperatively.11 Techniques as placement of haemostatic material at durotomy site have been cited previously,6 and since the chronically inflamed dura is friable, less manipulation can, at least theoretically, provide better results in such cases.
In conclusion, intradural disc prolapse is a rare presentation and the surgical excision of this entity is more cumbersome. Preoperative diagnosis is challenging and is rarely made. Spinal surgeons should be vigilant about this rare condition to manage it appropriately.
PATIENTS’ CONSENT:
Written, informed consents were taken from the patients to publish this case report.
COMPETING INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
ZM, MN, MU: Proposed the study, analysed the data, and prepared the final draft.
RA: Contibuted to the study design, data interpretation, and review of the final manuscript.
All authors approved the final version of the manuscript to be published.
REFERENCES